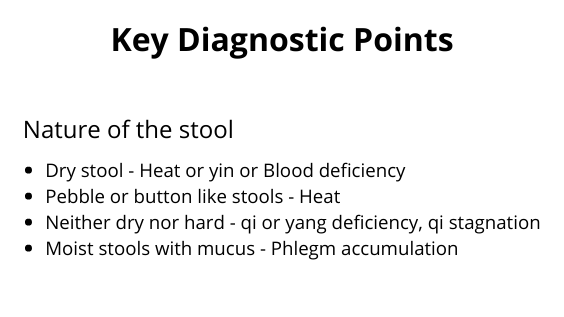
Constipation is difficulty in passing stools, prolonged intervals between stools, or a desire to defecate without the ability to do partially or completely. The stools may be hard, dry and pebble like, or essentially normal (this is, moist and well formed).
People have widely varying ideas as to what constitutes a normal bowel pattern. To some individuals, one motion per week is normal, while others consider themselves to be constipated if the defecate only once daily. In TCM the baseline for ‘normal’ is at least one unforced stool everyday or second day.
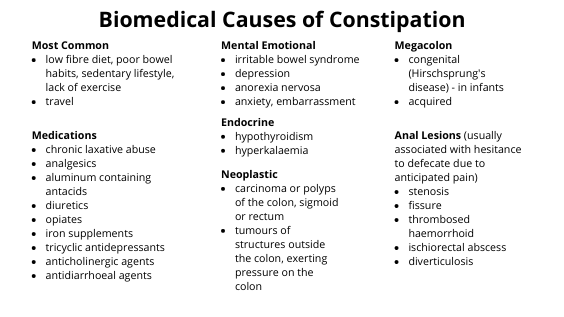
Constipation is a common problem, and in the western world appears to be largely related to diet and sedentary habits. Constipation can also an acute event associated with other primary illnesses, typically those characterised by fever or dehydration. In these situations however, the constipation itself is unlikely to be the presenting problem, although it will certainly be considered in the treatment strategy.
Constipation can be broadly divided into two types, excess and deficient. the excess patterns are characterised by the presence of a pathogen (typically Heat or Phlegm) or by pathological accumulation of qi that blocks the qi mechanism and the decent of Large Intestine qi. The deficient patterns are characterised by dryness from insufficient fluid lubrication in the form of body fluids, Blood or yin, or lack of propulsion through the digestive tract from deficiency of qi or yang.

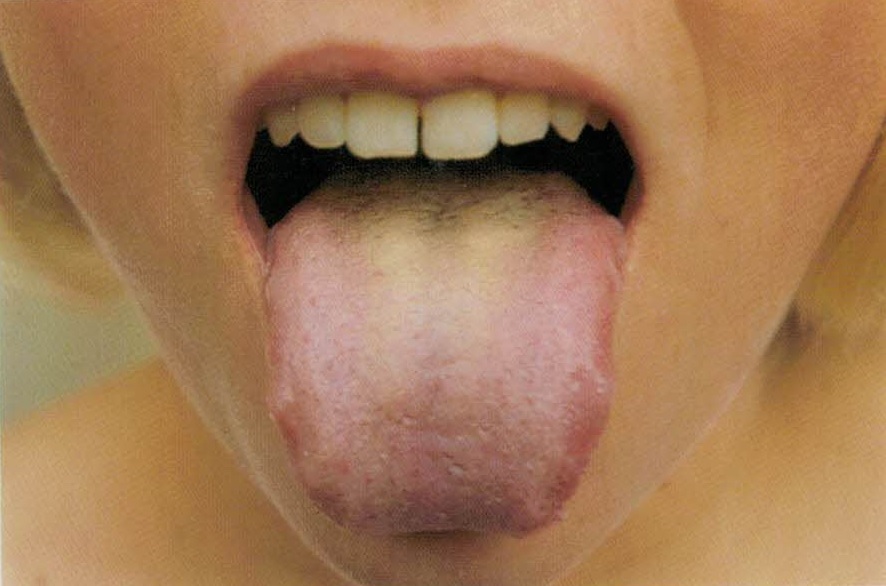
Heat
Heat causing constipation can be external or internal origin. When external Heat causes constipation, it may be systemic Heat (as in Heat in the Blood), or more commonly, Heat in the qi level, this is, Heat invasion of the Lungs and/or Stomach and Intestines.
External Heat
Heat in the Lungs
Invasion of an external Heat pathogen, or other pathogen which transforms into heat once the body, will dry body fluids and parch those parts of the body most sensitive to dryness, the Lungs and Intestines.
Heat in the Stomach and Intestines
Heat invasion of the Stomach and Large Intestine is described ad yang ming syndrome.
Internal Heat
The most common cause of internal Heat type constipation is diet (see below). Internal Heat can also be generated by prolonged frustration, resentment, or other emotional turmoil that impends the movement of Liver qi. The transformation of stagnant qi into Heat is aided by consumption of heating foods and beverages, especially alcohol, rich, fatty or supplementing foods. In addition, cigarette smoking, or working in a very dry or dehumidified environment can dry the Lungs, and by extension, the Large Intestine.
Diet
The type of food consumed and the way it is consumed are important factors in the genesis of constipation. the western diet is, for the most part, heavy in protein and fat, and light in dietary fibre. Dietary fibre, from the cell walls of grains, vegetables and fruits is largely composed of cellulose, and is indigestible in humans. Fibre acts as a bulking agent, increasing the volume of the stool, thus triggering the stretch receptors in the intestinal wall. This in turn stimulates intestinal peristalsis and decreases transit time of waste material through the intestine. Insufficient fibre and high proportion of fat, which slows transit time, contribute significantly to sluggish movement of waste material through the bowel, and thus constipation.
Emotion
The Stomach and Intestine rely on the smooth passage of Liver qi for their orderly function, and to some extent on the unimpeded descent of Lung qi. A combination of stress and inactivity or sedentary occupation which weakens Lung qi and causes a general sluggishness of qi, can lead to general derangement of gastrointestinal function.

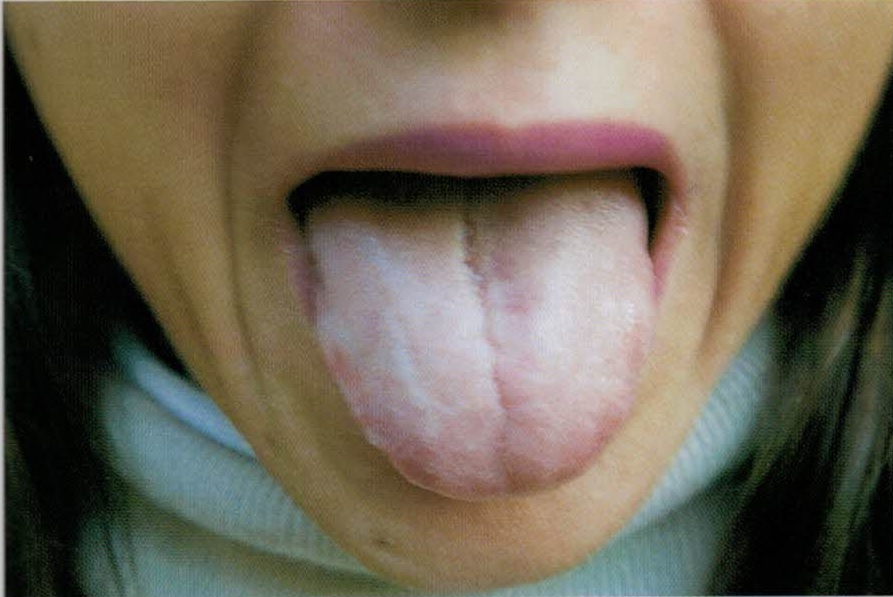
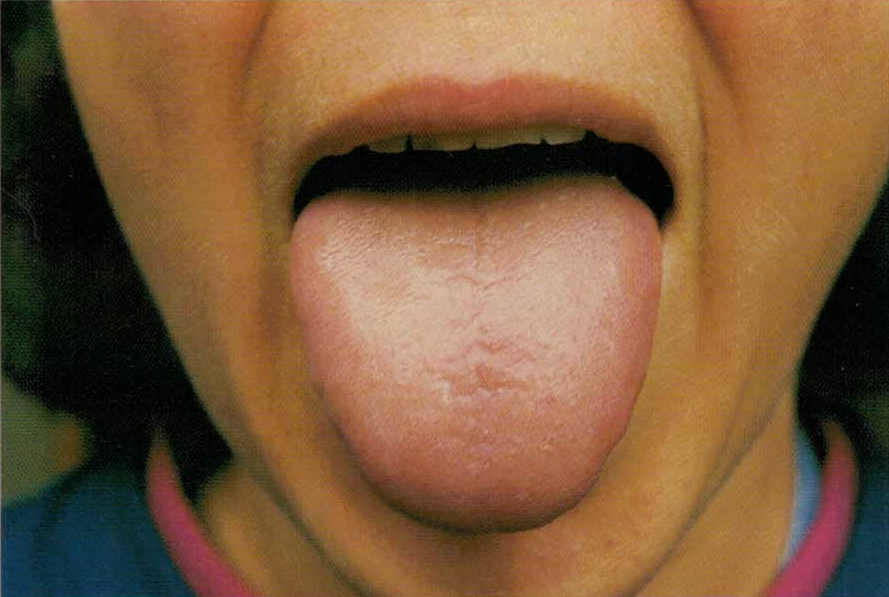
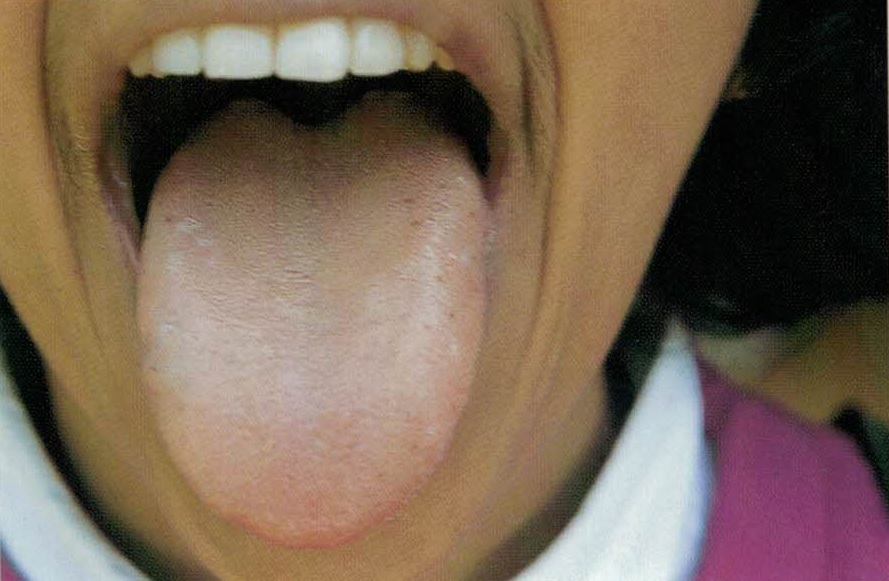
Yin, Blood and Fluid Deficiency
Yin, Blood and fluid deficiency patterns are very common causes of chronic constipation and are due to insufficient lubrication of the bowel by yin fluids, including Blood. Yin and Blood deficiency patterns frequently occur in elderly and postpartum patients because their yin is naturally depleted.
Qi and Yang Deficiency
Qi and yang deficiency types of constipation are due to a lack of qi movement in the Intestines, compounded in the case of yang deficiency by Cold which ‘freezes and constricts’ movement through the intestines, further slowing the passage of stools.
Lack of Exercise
Insufficient physical activity can contribute to constipation. People who sit all day tend to have systemically sluggish qi, which impends movement of qi and thus waste material through the Intestines. Similarly, lack of exercise weakens the Spleen and Lungs. When the Spleen is weak, the qi mechanism is easily disrupted, stomach qi fails to descend properly and qi movement through the abdomen slows.
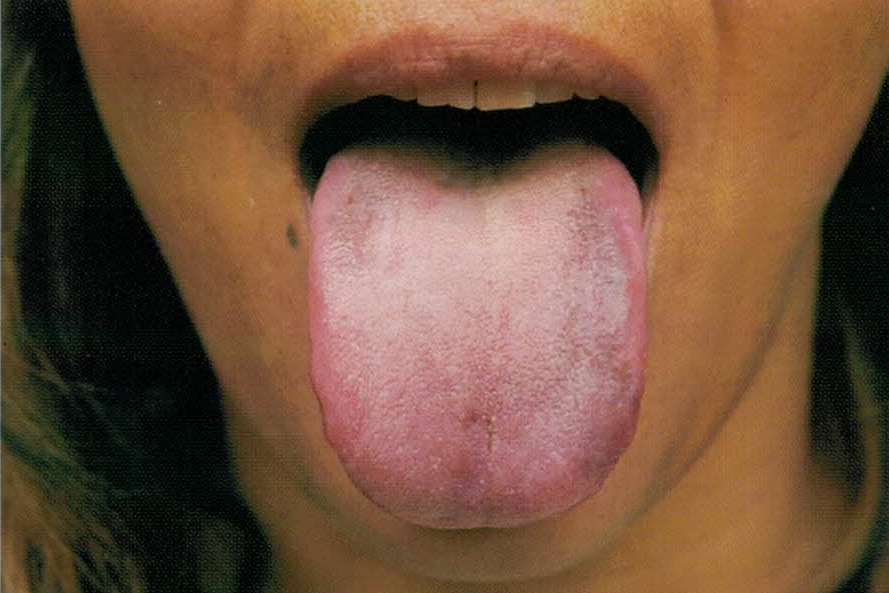
Diagnosis
Of the excess patterns, the most frequent cause of constipation in the western world is insufficient dietary fibre. With rich, high density, supplementing foods like fats and meat. colonic transit time is slowed and food stagnates.
Treatment
Traditional Chinese herbs and acupuncture can be useful in speeding recovery.