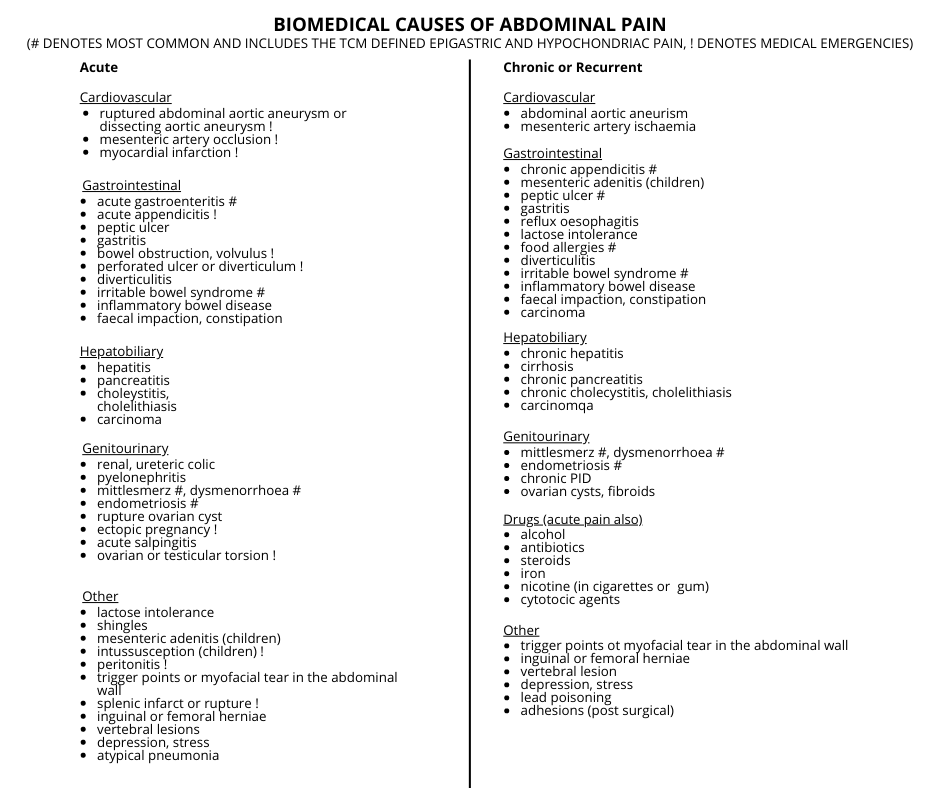
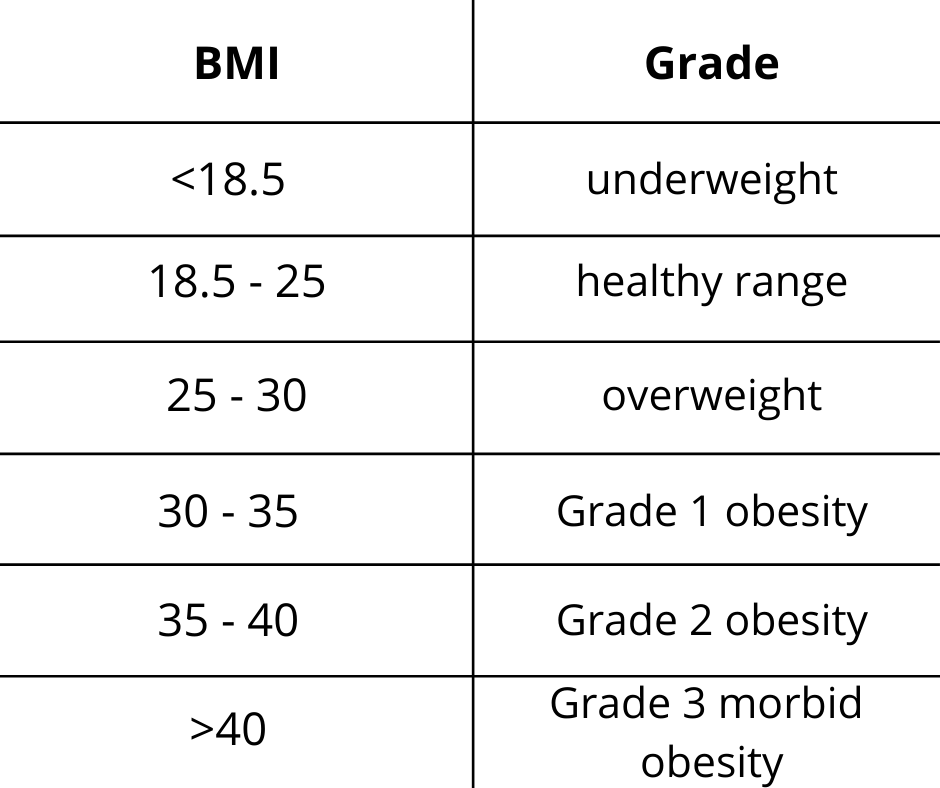
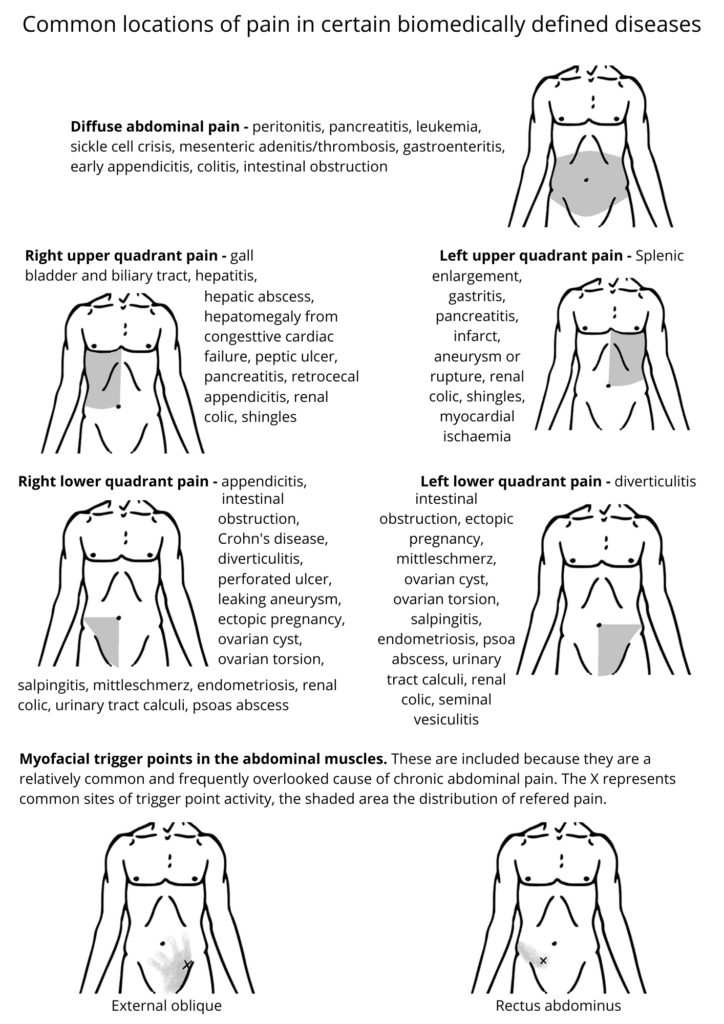
Abdominal pain is a common presenting symptom in the TCM clinic. The pain can be acute or chronic, diffuse or well localised. When acute and sever, surgical referral may be necessary. When analysing a patient with acute pain, it is important to keep in mind those conditions considered medical emergencies. Also note that textbook descriptions of pain are limited due to the different responses of individuals to pain. Obese and elderly patients tend to tolerate pain better than others, while in highly strung individuals the experience of pain may be magnified. Patients with chronic pain are most likely to seek TCM treatment. There are many biomedical causes of abdominal pain, many of which are amenable to TCM treatment.
Pain in TCM terms is always due to some impediment to the circulation of qi and Blood , hence the adage where there is obstruction there is pain, where there is no obstruction there is no pain. This important principle provides a guide for treatment of all types of pain. Pain can be broadly divided into two types – excess and deficient.
Excess pain is caused by the presence of a pathogen which physically obstructs qi and Blood flow. Any pathogen can hinder the flow of qi and Blood, but Cold, qi stagnation and Blood stagnation are the most likely to produce pain. The general principle of treatment for excess pain is to identify the obstructing pathogen and eliminate it.
Deficient pain is the result of insufficient motive force behind the circulation of low levels of qi and Blood, so that they become sluggish and begin to pool. This is likened to the stagnant pools that form in a riverbed as the water level drops during drought. Pain results, and the solution is to restore the qi, yang and Blood.
Cold
Cold is an extremely common cause of both acute and chronic abdominal pain, as the nature of cold is to ‘freeze and constrict’. By freezing and constricting abdominal structures, the circulation of qi and Blood is reduced and pain is easily produced.
External Cold
Cold can be introduced into the body by association with Wind, by ingesting cold foods or drinks, or by direct exposure of the body to cold. A common example of the latter is invasion of the Uterus by cold while swimming during menstruation. Cold has an affinity with both the Intestines and the Uterus, and in both cases cause quite severe cramping or colicky pain that is significantly alleviated by application of heat. External Cold may be associated with Dampness, or may transform into Heat pathogen once in the body.
Internal Cold
Internal Cold is the product of Spleen and/or Kidney yang deficiency patterns, where yin Cold becomes predominant relative to warming active yang. The manifestation of the pattern will vary depending on the degree of deficiency relative to the strength of the excess Cold. When the deficient aspects are dominant, the pain produced will be of a deficient Cold type (mild and dull, relieved by warmth and pressure). When yin Cold is ascendant, the pain will tend to be severe, relieved by warmth but worse with pressure. The background yang deficiency patterns are chronic conditions. Spleen yang is primarily weakened by diet. Weak Kidney yang or qi may be an inherited condition, or may develop as a result of age, chronic illness, too much exposure to cold conditions, or excessive lifting or standing. Kidney yang or qi may also be damaged by excessive or premature sexual activity (especially in men, but also women), or specifically in women by many pregnancies, miscarriages and/or terminations.
Heat
Heat that causes abdominal pain includes invasion of external Heat, external and internally generated Damp Heat, Toxic Heat and Summerheat.
External Heat
External Heat can invade directly into the Intestines, or transform from a Cold invasion (also known as yang ming fu syndrome). The Heat parches the Intestine and stool causing constipation and pain. External Damp Heat can invade the Intestines or Uterus. Damp Heat in the Intestines can be a product of the season, commonly occurring during hot or humid weather, and more common in tropical climates. Damp Heat pathogens can also invade with spoiled food, or by sudden overindulgence in Damp Hot substances, such as alcohol, fats, and greasy rich foods. Damp Heat in the Uterus can result from an external Damp Heat pathogens that invades through the tai yang (Urinary Bladder) channel, the leg yin channels or the local luo channels. In practice, transmission of Damp Heat through the luo channels is probably the most common mode of entry (especially in sexually active individuals). It also occurs in postpartum women due to their relative deficiency and thus their vulnerability to external invasion.
Internal Heat
Internally generated Heat or Damp Heat can also cause abdominal pain. Damp Heat generated in the middle jiao by over consumption of rich, greasy or spicy foods and alcohol can simply sink and settle in the intestines. Damp Heat can also be generated in the lower jiao by any prolonged Heat in the system, such as the deficient Heat arising from yin deficiency, the stagnant Heat from liver qi stagnation, prolonged stagnation of Dampness or transformation of Cold.
Emotion
Liver qi stagnation is caused by repressed emotion, frustration, anger and resentment. These emotions, especially when chronically unexpressed, cause a low grade spasm and tension in the smooth muscles of the gut – a classic emotional ‘holding pattern’. Patients with chronic qi stagnation type digestive problems will often note that their stress and tension is reflected in their gut and be aware of the consequences of stress – the knot in the stomach, cramps, loss of appetite, diarrhea etc. This type of abdominal pain tends to be intermittent and is clearly related to the emotional state. Prolonged qi stagnation can contribute to several complications which also cause pain – Blood stagnation, stagnant Heat and Spleen deficiency with the eventual generation of internal Cold or Phlegm Damp. In addition, qi stagnation leads to a generalized hyper toxicity of both skeletal and smooth muscle, further restricting the circulation of qi and Blood to the tissues.
Blood Stagnation
Blood stagnation type abdominal pain may be acute or chronic. Acute pain may follow abdominal trauma or surgery. Chronic pain follows some other prolonged disorder affecting the abdomen. Any pathology, excess or deficient, if long lasting enough, may lead to Blood stagnation. Cold pathologies (Cold and yang deficiency) can cause Blood stagnation by ‘freezing and constricting’ the vessels and slowing circulation of qi and Blood. Hot pathologies (Heat, Damp Heat, Phlegm Heat and yin deficiency) can cause stagnation by ‘evaporating’ Blood and increasing the viscosity and sickness of Blood. Chronic Liver qi stagnation fails to lead the Blood and is a very common precursor to Blood stagnation.
Diet
The type of food consumed and the way it is consumed are important factors in the genesis of abdominal pain. Eating spoiled or contaminated food can produce acute pain, which in TCM terms may resemble an invasion of external Cold Damp or Damp Heat. Too much cold natured or raw food can introduce Cold and weaken Spleen qi and yang. Some drugs weaken the Spleen and deplete Spleen and qi yang. These include purgative laxatives, antibiotics, non-steroidal anti inflammatory drugs (NSAIDs), and the anti-retroviral drugs and protein inhibitors used to treat HIV infection. Reduced food intake as a result of strict dieting, or prolonged starvation and digestive insult, seriously damages Spleen yang. This can occur in patients with history of anorexia nervosa, bulimia, or during famine. Over consumption in general, and excessive consumption of rich, heating or supplementing foods in particular, can lead to the accumulation of stagnant food and Heat or Damp Heat in the Stomach and Intestines. Food stagnation is a common precursor to a host of pathologies that may give rise to abdominal pain. An excess of heating foods, such as chilli, coffee, spirits, spices, fats and meat can introduce Heat and Damp, or damage yin. Sugar and dairy products create Dampness and Phlegm.
Treatment
TCM treatment of abdominal pain would start with the diagnoses of which of the above is causing the pain. Once the cause is identified, a combination of acupuncture and Chinese herbs will be prescribed.